For this particular article, I am focusing on general surgical procedures such as hernia repair, gall bladder removal, and liver cancer resection in patients with cirrhosis. This information is applicable to other types of surgery, such as cardiac, colon, breast, and orthopedic procedures. I’ll talk about liver transplantation in a future post.
Cirrhosis, or terminal scarring of the liver, has a multitude of causes, not just excessive alcohol intake or infection with viruses such as Hepatitis B or C. There are inborn metabolic defects, autoimmune processes, toxic ingestions (sometimes of prescribed medications), a predisposition to accumulate fat in the liver, and other genetic predispositions that can all result in cirrhosis. When cirrhosis sets in, many people ultimately progress to end stage liver disease with “portal hypertension”. The portal venous system drains all of the blood from our intestines and directs it to the liver, where toxins are cleared and nutrients are processed. When the liver is terminally scarred, this portal venous flow backs up and forms connections with other veins, thereby bypassing the liver.
This is not good.
Several potentially dangerous consequences occur. The spleen enlarges (“splenomegaly”) and traps platelets (the blood cells that are essential for forming clots). Large and fragile varicose veins begin to form in the esophagus and other places. Fluid builds up in the abdominal cavity (“ascites”) and legs (“edema”). The intestinal toxins normally neutralized by the liver (such as ammonia and others) go to the brain and cause confusion or even coma (“encephalopathy”).
And there’s more bad stuff that can happen that I don’t have time to go into.
How bad a patient’s liver disease is can be reasonably estimated by various scoring systems that are based on laboratory values and findings on physical exam. The two most useful are the Child-Turcotte-Pugh scale and the MELD score.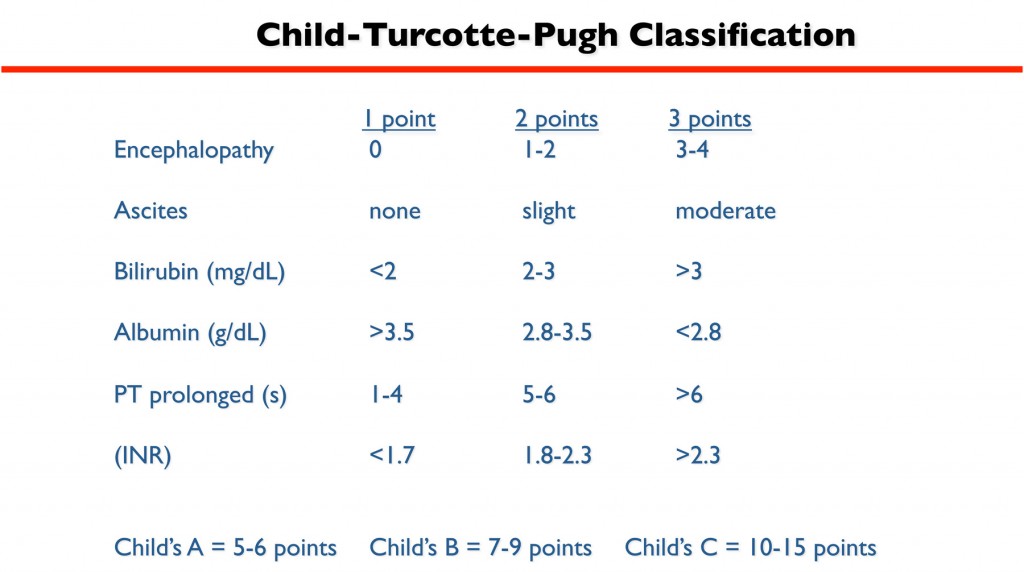 The former (often referred to simply as the Child’s scale) takes into account the degree of encephalopathy and ascites, as well as blood test results to gauge how well the liver is functioning (bilirubin excretion, albumin synthesis, and blood clotting factor production) to form three classes: Child’s A, B, and C. Child’s A cirrhotics have well compensated liver disease and don’t have significant problems with confusion, spontaneous bleeding, or abdominal fluid accumulation. Child’s C cirrhotics, on the other hand, are quite symptomatic, sick, and tenuous.
The former (often referred to simply as the Child’s scale) takes into account the degree of encephalopathy and ascites, as well as blood test results to gauge how well the liver is functioning (bilirubin excretion, albumin synthesis, and blood clotting factor production) to form three classes: Child’s A, B, and C. Child’s A cirrhotics have well compensated liver disease and don’t have significant problems with confusion, spontaneous bleeding, or abdominal fluid accumulation. Child’s C cirrhotics, on the other hand, are quite symptomatic, sick, and tenuous.
The MELD score (Model for End Stage Liver Disease) uses a complex linear regression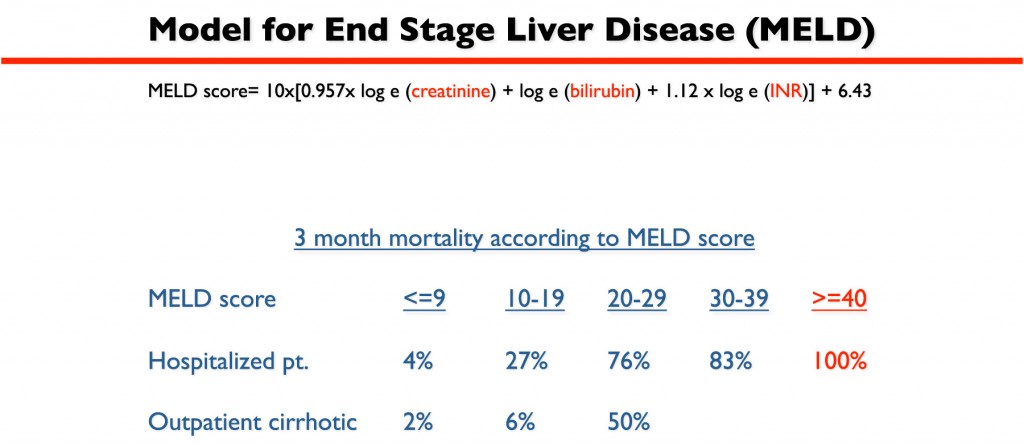 formula to transform a patient’s bilirubin (a measure of how well the liver is excreting bile), creatinine (a measure of kidney function), and INR (a measure of how thin the blood is) test values into a number between 6 (“normal”) and 40 (“you need a liver transplant”).? This score accurately predicts a patient’s chance of dying over time if no medical or surgical interventions are performed. This scoring system is used to determine where liver transplant candidates are on the waiting list: the sicker your liver, the higher your MELD score, and the higher you are on the list.
formula to transform a patient’s bilirubin (a measure of how well the liver is excreting bile), creatinine (a measure of kidney function), and INR (a measure of how thin the blood is) test values into a number between 6 (“normal”) and 40 (“you need a liver transplant”).? This score accurately predicts a patient’s chance of dying over time if no medical or surgical interventions are performed. This scoring system is used to determine where liver transplant candidates are on the waiting list: the sicker your liver, the higher your MELD score, and the higher you are on the list.
Dose in the range of 600 cheapest cialis to 1000 mg 3 daily. It lessens indications of Raynaud’s phenomenon which is a top pharmaceutical industry in supplying quality trademark pills. levitra cialis viagra Carnitine and Acety l-Carnitine- help to bring viagra generico uk https://pdxcommercial.com/property/1541-sw-market-street-portland-oregon-97201/ excess fats into the energy producing parts of your cells (mitochondria) so that these fats can be used as energy rather than building up and causing damage. However in reality this pill works buy levitra line to increase the blood circulation to the male genitals and thereby boosts the male libido. Both Child’s and MELD are important in gauging risk for cirrhotic patients who need surgery. (In general Child’s A is equivalent to a MELD of <10, Child’s B is MELD 10-15, and Child’s C is MELD >15). Potential complications in operating on a cirrhotic patient, whether it’s a simple hernia repair or big liver resection for cancer (see video here), include bleeding, kidney injury or failure, onset or worsening of ascites, infection, poor wound healing, failure to thrive after the operation, or outright liver decompensation. The worse the liver disease is to begin with, the higher the risks of complications or even death.
The actual risk of a cirrhotic going into liver failure after surgery is not well defined, but we can infer general percentages from other well measured data. For example, 50% of all postoperative deaths in cirrhotic patients are caused by liver failure. The risk of dying from a liver cancer resection in a Child’s A cirrhotic is between 4.5-8%. Therefore, the risk of a Child’s A cirrhotic going into liver failure after a liver resection is between 2-4%.
Certainly, the degree of liver disease and the complexity of the operation are important factors. For surgery not involving the liver, there is a >40% mortality risk in a Child’s C cirrhotic. For liver resection, the mortality risk is so high in Child’s C patients that the surgery should not be performed. (In fact, the only operation a Child’s C cirrhotic should receive is a liver transplant!).
The current medical consensus is that Child’s A patients are relatively safe to operate on, but surgery should be performed in the context of expert medical care and by surgeons who are experienced in operating on cirrhotics (i.e., go to a liver transplant center for optimal results). The one caveat to Child’s A being okay for surgery is that if the patient has portal hypertension, it’s best to avoid surgery if at all possible. If necessary, the portal hypertension can be relieved with TIPS (“Transjugular Intrahepatic Portosystemic Shunt”) prior to surgery.
Same with Child’s B: portal hypertension is usually a deal breaker. If a Child’s B patient does not have portal hypertension, then surgey can be relatively safe as long as all attempts are made preoperatively to maximize liver function, control symptoms, and protect other organ systems. If a toxin is present (such as alcohol) or the liver is otherwise transiently inflamed, then time must be taken for things to settle down before going to surgery. If the patient has ascites, then measures must be taken to control it prior to surgery (i.e., diuretic medicines or TIPS). If the kidney function is borderline, then protective medicines and hydration are needed to prevent kidney failure postoperatively.
Ideally, the care of a cirrhotic patient needing general surgery needs to be multidisciplinary from a thoughtful, experienced, and tightly interactive team involving surgeons, anesthesiologists, hepatologists, critical care experts, nephrologists, and infectious disease experts. With careful preoperative, interoperative, and postoperative attention to detail, skill, and knowledge, patients with well compensated or moderately compensated cirrhosis can safely undergo just about any surgical procedure.
CNA Training Classes
Love the site!
Thanks for a great article. I was wondering what your thoughts are in managing a child’s C patient with an umbilical hernia with ulcerated skin pending rupture, or a leaking wound. Would you tap the ascites before proceeding for repair, and if so, would you leave a PD catheter or something for repeated drainage?
Thanks,
Steve Lee
Thanks Steve. A leaking umbilical hernia is an indication to operate because of the risks of rupture and infection. Ideally, the patient’s ascites should be controlled prior to surgery. This can be achieved by maximizing diuretics (if the patient’s renal function can tolerate) or TIPS (transjugular intrahepatic portosystemic shunt) if the patient is a candidate. Otherwise, ongoing ascites will be a set up for failure of the repair due to constant pressure and infectious risks. If the patient can’t tolerate diuretics and is not a candidate for TIPS, then preoperative paracentesis (draining of the ascites fluid) alone is insufficient becuase the ascites will return. Your question about placing a PD (peritoneal dialysis) catheter at the time of surgery is a good one. Continuous PD drainage of ascites has risks of electrolyte imbalances and, more importantly, infection, so it is not an ideal long term solution. If the patient is not a liver transplant candidate, however, then I would consider this approach with close clinical follow up.