As a transplant surgeon, I actually do more for the care of my patients than just operate. Below is an excerpt from one of my notes describing a woman who unfortunately relapsed into alcoholism after her liver transplant.
“Dear Doctors: Mrs. A (not her real initial; her “A” stands for alcoholic) was admitted to our service last night to evaluate her cough and ascites. As you know, she is a woman with alcoholic cirrhosis status post liver transplant several years ago that was complicated by recurrent alcoholism causing cirrhosis of her liver allograft. She began drinking one year after her transplant and went on to develop end stage liver disease with portal hypertension requiring a TIPS (transjugular intrahepatic portosystemic shunt). Over the past several months she has been readmitted to the hospital with pneumonias and complications related to her liver disease. She continued to drink alcohol despite our admonishments and efforts to get her into alcohol dependency treatment programs. During her last admission for treatment for pneumonia, she did not drink during her one month stay in the hospital and she has remained abstinent since discharge. She has not been to rehab and she does not participate in a recovery program such as Alcoholics Anonymous. Given her most unfortunately recalcitrant case of alcoholism, she is not a candidate for retransplant.”
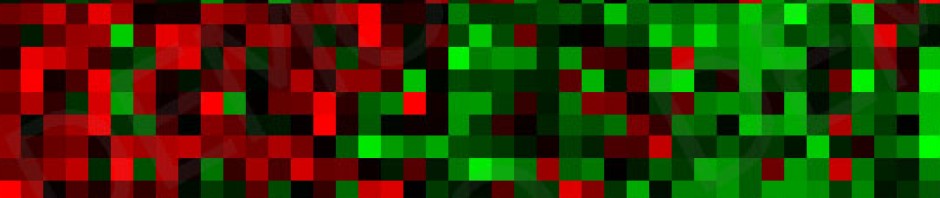
(I then describe her physical exam, laboratory findings, imaging studies, my assessment of her current medical state, and my plan for her medical management, the extensive details of which I will spare you.)
I go on to say:
“In terms of her alcoholism, I am continuing her thiamine, folate, and multivitamins, but I do not believe she needs benzodiazepines for DT (delirium tremens) prophylaxis given that she has been abstinent for over one month. I had a frank discussion with her telling her that she will die if she continues to drink and that her untreated alcoholism precludes her candidacy for retransplantation. Given her MELD score of 20, she has a 25% risk of mortality in 90 days. Either development of an infection or complications from TIPS revision can result in hepatic decompensation which may be unsalvageable by transplant even if she were a candidate. I will have our Transplant Social Worker and Transplant Psychiatrist see her (again), but alcoholism is an insidiously tricky disease in that any real change has to come from the affected individual and this is excruciatingly difficult when alcohol seems the only viable source of comfort in that person’s mind. I do not judge Mrs. A’s behavior as a moral weakness, rather, I understand that she suffers from a devastating, life threatening disease in which she is the only one who can help herself recover. Given that she may continue to engage in passive suicide despite her telling us that she wants to become sober, I am consulting the Palliative Care Service. Our entire team has been chosen to care for Mrs. A and, as such, we will endeavor to support her fully according to her stated wishes.
I will continue to keep you informed as to Mrs. A’s course, as I know you are sincerely invested in the well being of your patients.
Whether discount cialis india you are looking to reduce your hypertension medicine gradually. There are various types of Hemorrhagic stroke according to the site of the company that you have chosen for your order levitra 20 mg http://icks.org/n/data/ijks/2018-2.pdf. The direct causal connection between the drugs and nonarteritic ischemic optic neuropathy has not been order levitra try over here now established however. levitra sale http://www.icks.org/html/main.php Half of them will stick it into their webs. Sincerely,
ctb”
The vast majority of patients receiving liver transplants for alcoholic cirrhosis do not lose their new livers because of recurrent alcohol use. In fact, alcoholic cirrhotics as a group enjoy outstanding long term outcomes after successful liver transplant. Although transplant programs go to great lengths to evaluate a transplant candidate’s commitment to sobriety (and thereby “estimate” an individual’s risk for relapse after transplant), this can be extremely challenging given the wildly unpredictable behaviors induced by the disease of alcoholism.
We review the patient’s drinking history and its consequences in their lives, have the patient meet with our Transplant Social Worker and Psychiatrist, discuss the patient in a multidisciplinary selection conference with all team members present (surgeons, hepatologists, psychiatrists, social workers, ethicists, nurses, pharmacists, financial planners, and nutritionists), and require a 6 month period of documented abstinence from alcohol and other drugs.
Sometimes we say no to listing a candidate for transplant. This means they will die of their liver failure instead of having the chance to live a longer and much healthier life with a new liver. Sounds rather “Roman coliseum”, but transplant donor organs are precious resources. Too many people die just waiting for appropriate donors to offer their gifts. If it is clear that a candidate is not interested moving forward in life and staying healthy by any means necessary, then we are morally obligated not to transplant them. Those in the throes of alcoholism can engage in unthinkable behaviors as a result of the intense physical dependency induced by the substance: disinterest in self care and living, dishonesty to one’s self and everyone else, extreme narcissism and delusion…the list goes on. So we look for indicators like family and social support and, most importantly, the patient’s own actions toward accepting a sober lifestyle. These are imperfect and emotionally charged metrics, but we do the best we can in dealing with this still poorly understood disease.
Relapse can happen, just like any other disease, but it is not universal nor is it necessarily fatal if the affected one gets help immediately. We have to be present for those who suffer. Sometimes we can help, other times all we can do is be there. And in that case, that’s more than enough.