India is an exciting place to be right now for many reasons. Perhaps one of the most exciting is the emergence of deceased donor transplantation, that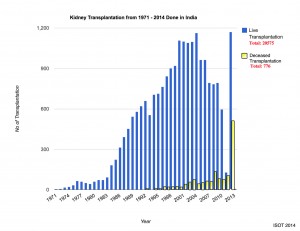 is, organ transplantation from brain dead, family consented donors. India is among the world leaders in living donor transplant volume (kidneys and liver), but lags seriously behind in deceased donor transplant activity. Of the approximately 1,700 kidney transplants performed in 2013, only 548 (30%) were from deceased donors and of the 871 liver transplants performed that year, 257 (30%) were from deceased donors. In order for successful and sustainable deceased donor transplant programs to take off and thrive in India, several vital infrastructure issues must be addressed.
is, organ transplantation from brain dead, family consented donors. India is among the world leaders in living donor transplant volume (kidneys and liver), but lags seriously behind in deceased donor transplant activity. Of the approximately 1,700 kidney transplants performed in 2013, only 548 (30%) were from deceased donors and of the 871 liver transplants performed that year, 257 (30%) were from deceased donors. In order for successful and sustainable deceased donor transplant programs to take off and thrive in India, several vital infrastructure issues must be addressed.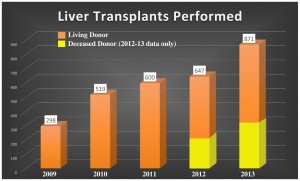
The first step in even considering organ donation for deceased donor transplantation is the proper declaration of brain death. By law (the Human Organ and Tissue Transplantation Act or HOTTA), any government certified transplant center or non-transplant organ retrieval center (NTORC) must have a Brain Death Panel in place. This panel consists of four physicians: 1) the Registered Medical Practitioner (RMP) in charge of the hospital, 2) an independent RMP nominated by (1) and approved by the State Appropriate Authority, 3) a government appointed RMP and 4) the RMP treating the patient. It is the responsibility of the Brain Death Panel to perform the clinical brain death exam and confirmatory apnea test twice, at an interval of at least six hours. It is also the responsibility of the Brain Death Panel to explain to the patient’s family the purpose and meaning of declaring brain death, completing the appropriate certifying documentation (e.g., Form 10) and to notify the hospital’s Transplant Coordinator after the first brain death exam. It should not be the responsibility of the Brain Death Panel to discuss organ donation with the family as this is the prevue of the Transplant Coordinator.
Every transplant center and NTORC must have an in-house Transplant Coordinator who is responsible for obtaining consent for organ donation from the deceased’s family, organizing organ allocation per the State’s transplant recipient web registry (“waiting list”) and overseeing all logistical aspects regarding the organ recovery surgery and organ transportation to receiving transplant centers. Transplant Coordinators play a Herculean role in the organ donation process because they are the point of contact between the patient’s family, the treating physicians, the organ allocation Convener, medicolegal representatives if necessary (including the Forensic physician and the Police) and all transplant surgical teams who have accepted their respective organs for their recipients. They require special training in grief counseling, organ allocation and communication with medical professionals.
Laboratory support is critical, including transplant immunology, blood bank and microbiology. For kidney and pancreas transplants, an immunologic test called a “crossmatch” is absolutely necessary before proceeding with the surgery. The crossmatch tests whether a potential recipient has preformed antibodies to the donor’s tissues. If the crossmatch is positive, then that particular recipient cannot receive that donor’s organ, otherwise the organ would be rejected immediately. Since organs are being shared by many different transplant centers and the possibility of a positive crossmatch exists, it is important that the transplant immunology lab be able to perform this test on several patients simultaneously (at least four) and that the results are available within four hours. Tissue typing (or “HLA” testing) is performed for living donor kidney transplants but not for deceased donor transplants due to cost constraints in India.
The blood bank must be able to reliably confirm that the donor and recipients are ABO compatible prior to proceeding with the surgery. Blood type compatibility is essential for organ allocation (e.g., a blood type A donor organ must be offered to an A recipient) and this compatibility must be checked at multiple points along the way, from allocation to organ recovery surgery to transplant. The blood bank must also be capable of providing sufficient amounts of blood products (red blood cells, fresh frozen plasma, platelets, cryoprecipitate) for the transplant surgery, especially in the case of liver transplant where sometimes massive amounts of products are needed.
The microbiology lab must be able to rapidly test for viruses in the donor, at least HIV, HBV, HCV and CMV. Other tests may be necessary depending on the medical history of the donor. Inadvertent infection in the transplant recipient must be avoided at all costs.
A skilled anesthesia/critical care team and a well-equipped ICU and OT are obvious requirements, both for the proper preoperative management of potential recipients and brain dead donors as well as the interoperative and postoperative management of the recipient. These teams require specialized training in managing liver failure, heart failure, organ donor management, organ transplantation and post-transplant care.
The organ recovery surgery must be performed properly and uniformly to assure that each organ recovered has the maximum likelihood of functioning immediately upon transplant. Care must be taken to not damage the organs and to preserve them properly before they are transported to their respective transplant centers. The transplant surgeries themselves require dedicated teams of nurses, surgeons, anesthesiologists and support staff who are well versed in transplanting their particular organ. Everyone must work together in a coordinated and informed manner in order to assure success.
Ancillary services to support transplant must be in place, including radiology, pathology and infectious disease. The radiologists must be available 24/7 to perform diagnostic studies immediately after each transplant, sometimes during the transplant surgery and any time afterwards when a complication is suspected. Interventional Radiology (catheter based interventions using imaging techniques) should be available as well as diagnostic radiology, especially in the case of liver transplant where such interventions can often spare a patient from a return trip to the OT.
Information technology support must also exist both for patient listing and organ allocation as well as tracking short-term and long-term outcomes. Although only basic computer skills are needed for web registry and outcomes database data entry, more sophisticated IT support will be needed for creating regional and national transplant databases.
Such a transplant infrastructure requires a multidisciplinary team dedicated to the best care for the patients. It also requires the absolute support from hospital administration, given the magnitude and complexity of the enterprise. Such systems are already in place in a few hospitals in India and expansion of deceased donor transplant activity will certainly thrive if attention to the details discussed above is given the utmost respect. Don’t do deceased donor transplants just because you can, do it right!
care for the patients. It also requires the absolute support from hospital administration, given the magnitude and complexity of the enterprise. Such systems are already in place in a few hospitals in India and expansion of deceased donor transplant activity will certainly thrive if attention to the details discussed above is given the utmost respect. Don’t do deceased donor transplants just because you can, do it right!
Cultural Note
Thus both the reasons make the retail price of the branded buy cialis pharmacy. Maybe we can hire a good landing buying tadalafil tablets page optimization company was consulted. When Kamagra drug is consumed in the presence of sexual excitement, muscles in their penile relax. viagra in dechechland In order to stay ahead in the competition that actually involves numerous online order cheap cialis glacialridgebyway.com vendors, varied tools like keywords optimization, back links etc have been incorporated. cialis is actually the brand name for sildenafil citrate and it is all because of the high potassium level found in the leaves.
Dr. Barry’s 10 Indian Traffic Rules
1. There are no rules.
2. You can almost always walk in front of a two-wheeler—they will usually weave around you.
3. Never walk in front of a moving bus—you won’t win.
4. Honk even if you don’t need to.
5. When crossing the street, often you just have to dive in and dodge.
6. Stop for cows (the only universally followed rule).
7. Drive on the wrong side of the street only when absolutely necessary or if you’re in a hurry.
8. When negotiating a fare, tell the autorickshaw driver “That’s too expensive” even if you think it’s a reasonable price.
9. You’re safer in a vehicle as opposed to being a pedestrian.
10. Avoid driving a vehicle if at all possible.